Haemorrhoids (UK spelling) or Hemorrhoids (US spelling), also known as piles, are swollen veins in the lower rectum and anus.
They are the result of increased pressure exerted in the rectal area, generally caused by straining during bowel movements, obesity, sitting for long periods of time, regular heavy lifting or pregnancy and childbirth.
Prolapsed haemorrhoids are a common, yet uncomfortable condition that affects millions of people worldwide. It is estimated that every year, nearly 5 million people in the UK experience the symptoms of haemorrhoids, which include itching, discomfort, bleeding, and even prolapse. While many people can manage the symptoms with lifestyle changes and over-the-counter treatments from their pharmacy, prolapsed haemorrhoids can be more severe and often require medical attention. But is surgery necessary for prolapsed haemorrhoids? And if not, what are the alternative treatment options available?
Let’s start with what prolapsed haemorrhoids are, how and why they occur, what to look out for, and how to manage the condition.
Please skip to section:
What are prolapsed haemorrhoids?
Why do haemorrhoids prolapse?
The different types & severity of haemorrhoids
Signs of prolapsed haemorrhoids
What are the treatment options for someone with prolapsed haemorrhoids?
How to treat prolapsed haemorrhoids at home?
Do I need surgery to get rid of prolapsed haemorrhoids?
What does eXroid® electrotherapy treatment involve?
What are prolapsed haemorrhoids?
Haemorrhoids can be internal (inside the rectum) or external (outside the anus). Internal haemorrhoids are usually not visible or felt, while external haemorrhoids are visible and can cause a lot of discomfort. When internal haemorrhoids become enlarged, they can prolapse, or protrude, outside the anus. This is known as a prolapsed internal haemorrhoid. In more severe cases, the haemorrhoid may become thrombosed, or filled with blood and clotted. If left untreated, these types of haemorrhoids can become quite large and cause significant pain.
Why do haemorrhoids prolapse?
There are several reasons why haemorrhoids prolapse, including:
Increased pressure in the anal or rectal area
Weakened tissue in the anal or rectal area
Inadequate lubrication during bowel movements.
Increased pressure in the anal or rectal area can cause the veins to swell, leading to the formation of haemorrhoids. This pressure can be caused by straining during bowel movements, pregnancy, or obesity. When the pressure becomes too great, the veins and associated tissues enlarge, allowing the haemorrhoids to protrude out of the anus.
Weakened tissue in the anal or rectal area can also lead to haemorrhoids prolapsing. This weakened tissue can be caused by aging, injury, or childbirth. As the tissue weakens, it becomes easier for the veins to swell and protrude out of the anus.
Inadequate lubrication during bowel movements can also lead to haemorrhoids prolapsing. When a person is constipated the stool can be very hard, making it difficult for the anus to open and close properly. This difficulty results in straining and this action can cause the veins and the associated support tissues to swell, leading to the formation of haemorrhoids. Additionally, not enough lubrication can cause the haemorrhoids to increasingly engorge, getting larger, making it easier for them to protrude out of the anus.
| If you would like to discuss your condition with our Patient Services team, why not call us now on 0800 999 3777 or click here for more contact options. |
The different types & severity of haemorrhoids
Prolapsed haemorrhoids, although they protrude out of the anus and thus appearing externally, they are medically categorised as an internal haemorrhoid. To help you understand a little more about the different types of haemorrhoids and how they may affect your life, we’ve explained the difference and what to look out for:
Internal haemorrhoids are located inside the anal canal and are generally not visible. They can cause rectal bleeding, itching, and discomfort. They are graded on a scale of 1-4 based on their size and symptoms.
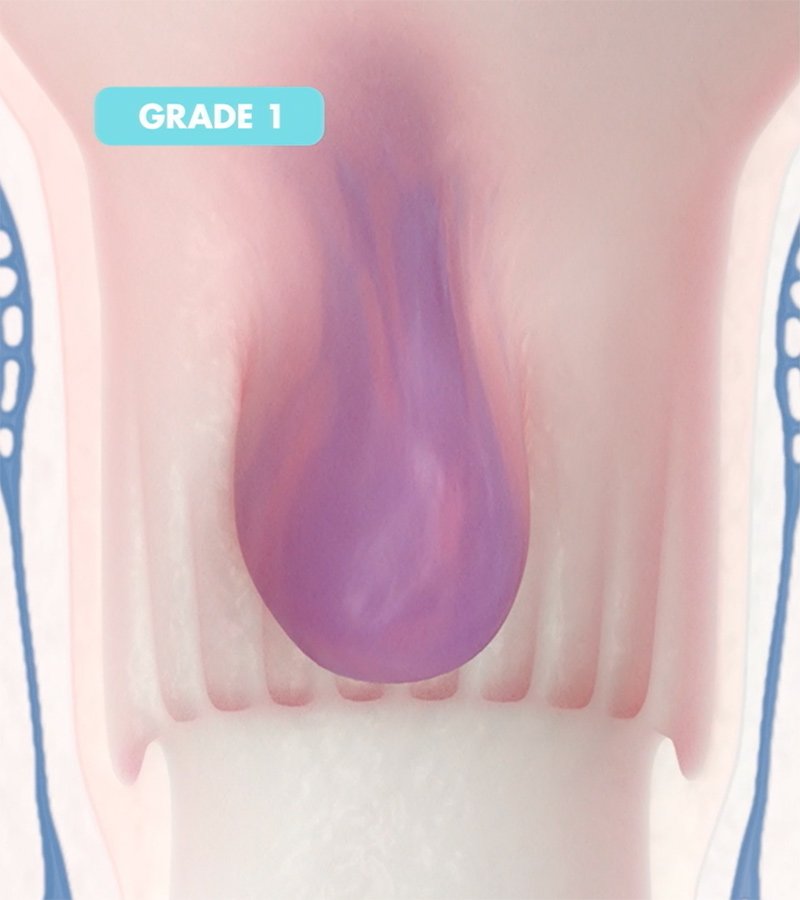
GRADE 1
Grade 1 haemorrhoids are internal haemorrhoids that are enlarged but remain inside the rectum
GRADE 2
Internal haemorrhoids that prolapse outside of the anus but spontaneously reduce on their own.
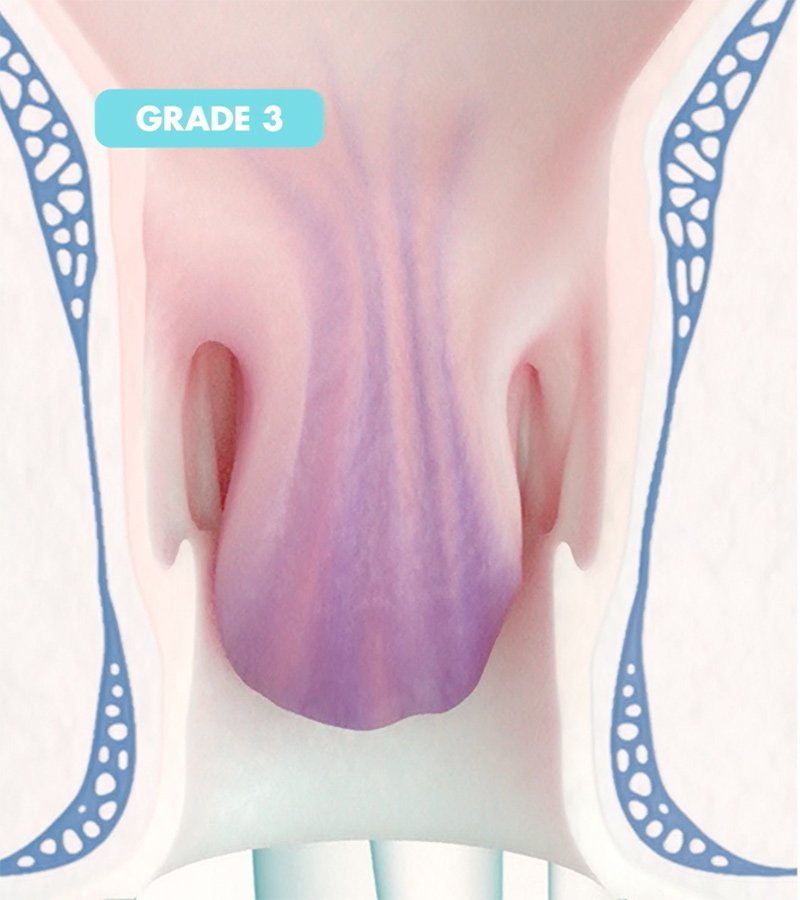
GRADE 3
Internal haemorrhoids that prolapse outside of the anus but must be manually pushed back in.
GRADE 4
Internal haemorrhoids that are permanently prolapsed outside of the anus and cannot be manually pushed back in.
External haemorrhoids are located outside the anus and are visible. They can cause pain and itching and can often develop a blood clot, also called a thrombosed haemorrhoid. These can cause significant pain initially, but they do generally improve spontaneously over a few days to a few weeks. Topical treatments and analgesia can ease the symptoms and allow more rapid resolution.
Internal and external haemorrhoids are both swollen veins in the lower rectum and anus but differ in their location and symptoms. Internal haemorrhoids are graded on a scale of 1-4 based on size and their propensity to protrusion, while external haemorrhoids can lead to a painful blood clot on the outside of the anus. This is usually caused by minor trauma, leading to the blood vessel bursting under the skin releasing blood which then clots, forming a painful and tender palpable lump.
Signs of prolapsed haemorrhoids
The most common symptom of prolapsed haemorrhoids is a lump or bulge that protrudes from the anus (not to be mistaken for sentinel piles, usually when having the bowels open, or when straining in other ways such as heavy lifting.
Other symptoms may include:
Painful bowel movements
Itching or irritation around the anus
Bleeding from the anus
A feeling of incomplete evacuation after a bowel movement
A feeling of fullness in the rectum
Mucus discharge from the anus
Swelling, inflammation, and tenderness in the rectal area
If you experience any of the above symptoms, it is important to see your doctor. A doctor can examine the area and provide the proper diagnosis and treatment. Treatment options vary depending on the severity of the prolapse and may include medications, lifestyle changes, minimally invasive procedures, or surgery.
What are the treatment options for someone with prolapsed haemorrhoids?
There are a number of treatment options for haemorrhoid sufferers to consider, whether that be to help relieve mild to moderate symptoms during a flare-up or to have a medical treatment to remove or reduce the cause of the symptoms, the haemorrhoids themselves, thus improving the impact and severity of the associated symptoms.
Treatment options include:
Lifestyle changes, including increasing fibre in the diet, drinking plenty of fluids, and avoiding straining during bowel movements.
Topical creams and ointments, which can help reduce inflammation and discomfort.
Medications, such as stool softeners and topical corticosteroids, to help reduce inflammation and pain.
Laser therapy, radiofrequency or infrared coagulation, which can help shrink the haemorrhoid.
eXroid® electrotherapy, which uses low-level electric current to shrink the haemorrhoid.
Sclerotherapy, which involves injecting a chemical solution into the haemorrhoid tissue to reduce swelling and bleeding.
Rubber band ligation (RBL) can also result in the removal of the haemorrhoid.
Surgical procedures, include haemorrhoidal artery ligation procedures (including HALO or THD), procedure for prolapsing haemorrhoids (PPH or stapling) and haemorrhoidectomy.
Haemorrhoidectomy is a surgical procedure where the haemorrhoid tissue is cut away and the remaining skin is either stitched back together or left to heal naturally.
| If you would like to discuss your condition with our Patient Services team, why not call us now on 0800 999 3777 or click here for more contact options. |
How to treat prolapsed haemorrhoids at home
The first step in treating prolapsed haemorrhoids is to make lifestyle changes to reduce your risk of developing them in the first place. This includes eating a healthy, low-fat diet high in fibre, drinking plenty of water, and exercising regularly. Additionally, it is important to avoid straining when having a bowel movement as this can exacerbate the condition. If lifestyle changes are not enough to reduce the pain and discomfort caused by prolapsed haemorrhoids, there are a variety of home remedies that can be used to help relieve the symptoms of prolapsed haemorrhoids.
At-home remedies for prolapsed haemorrhoid relief:
Take a warm bath or sue a Sitz bath with Epsom salt several times a day. This can help reduce inflammation and soothe the area.
Apply a cold compress to the area for 10-15 minutes several times a day.
Use a donut-shaped cushion when sitting to reduce pressure on the area.
Try to avoid sitting or standing for long periods of time.
Use an over-the-counter haemorrhoid cream or suppository to relieve symptoms.
Over-the-counter topical treatments for prolapsed haemorrhoids
The type of treatment used will depend on the severity of the symptoms. For prolapsed haemorrhoids, the most common form of treatment is topical ointments or creams, which can be purchased over the counter or with a prescription. These ointments can be applied directly to the affected area to reduce swelling, itching, and discomfort.
Try starting with a topical ointment or cream, such as those containing hydrocortisone, zinc oxide, or lidocaine, to help reduce swelling and pain. We also suggest you look for products containing natural ingredients like aloe vera and witch hazel, as these may provide additional relief. Over-the-counter suppositories are also available. These are inserted into the rectum, where they help to reduce inflammation, swelling, and irritation. Some medications, such as laxatives and stool softeners, can also help to reduce the pain and discomfort caused by prolapsed haemorrhoids.
If you find that the topical treatment isn't working, or if your symptoms are severe, you may need to consider a prescription topical cream or ointment. Your doctor may prescribe topical steroids or other medications to reduce inflammation and discomfort. If you have any additional questions or concerns, please don't hesitate to ask your pharmacist or doctor.
In cases where lifestyle changes and other treatments do not provide relief, medical treatment may be necessary to remove or shrink the haemorrhoids themselves.
Do I need surgery to get rid of prolapsed haemorrhoids
It depends on the severity of the prolapsed haemorrhoids. In some cases, conservative treatments such as lifestyle changes, dietary modifications, and topical medications may be enough to reduce symptoms. When they are not, non-surgical treatments and procedures can be used to reduce the severity of haemorrhoids without the need for surgery.
Non-surgical treatments are often performed in outpatient clinics without anaesthesia, making for a more convenient and lower risk treatment. Where haemorrhoid sufferers find little improvement with conservative therapy, non-surgical treatments have been widely effective for patients suffering bleeding and prolapse caused by early haemorrhoidal stages.
The most common non-surgical treatments for haemorrhoids:
Rubber Band Ligation (RBL or banding): A rubber band is placed around the base of the haemorrhoid, cutting off its blood supply. This makes the haemorrhoid shrink and eventually fall off.
Haemorrhoid Sclerotherapy: This involves injecting a chemical solution into the haemorrhoid to make it shrink.
Haemorrhoid Infrared Coagulation, Laser Treatment and Radiofrequency all generate heat: The heat generated using these different devices can seal off the blood vessels supplying the haemorrhoid, thereby reducing them.
Direct Current Electrotherapy: The eXroid® electrotherapy procedure is a non-surgical, minimally invasive treatment for haemorrhoids that uses direct current electrotherapy to stimulate the production of hydroxide ions that causes chemical cauterisation resulting in a reduction in the size of the haemorrhoids (this is not a heat treatment).
What does eXroid® electrotherapy treatment involve?
eXroid® is an electrotherapy procedure for the treatment of haemorrhoids. It involves the use of a small probe inserted into the anal canal, which is then gently rested onto the rectal mucosa at the point where the feeding vessels to the haemorrhoid are situated. It then uses direct current electrotherapy to reduce the size of the haemorrhoids by starving the blood supply feeding into the haemorrhoid. The procedure is minimally invasive and can be done in a clinic setting in less than an hour, with minimal discomfort. The eXroid® procedure is safe and effective and is an excellent alternative to more invasive surgical treatments.
It can be used for all 4 grades of internal haemorrhoids and is the only non-surgical treatment that can do this.
Watch our explainer video for more information
Surgery can be invasive and can cause further complications, so non-surgical treatments should be attempted first. If non-surgical treatments are not effective, then surgery may be an option.
Our expert team are on-hand to offer impartial and friendly advice, from booking an examination to helping you decide which treatment option is best for you, whether that be the eXroid® treatment or not.
Call us on 0800 999 3777 or click here for all other queries.
Would you like to discuss your condition with a trained advisor?
Please call us now on 0800 999 3777 or let us know your contact details below and we'll be in touch:Want to understand your haemorrhoid symptoms better?
Answer some simple questions about the symptoms you are experiencing to get your haemorrhoid severity score and receive advice on what it means and what to do next.